Inverell resident Darren Beetson knows when he goes to bed, it will be another unsuccessful attempt to sleep through the night. The 30-year-old suffers chronic pain in his shoulder from a motorbike accident and in his back which he hurt at work 2 years ago; the pain is so severe he can’t sleep without medication.
“Sometimes I just wake up and my shoulder has dislocated itself and I can’t get back to sleep. It’s agonising, pretty much the only word for it,” he says.
Beetson was living in Brisbane until 12 months ago when he moved to Inverell with his family. His doctor in Brisbane was able to prescribe him Codeine and Lyrica to help with the pain while he waits for surgery on his left shoulder. But not long after he moved, he was forced to withdraw from both, unable to get access to the medication in his new town.
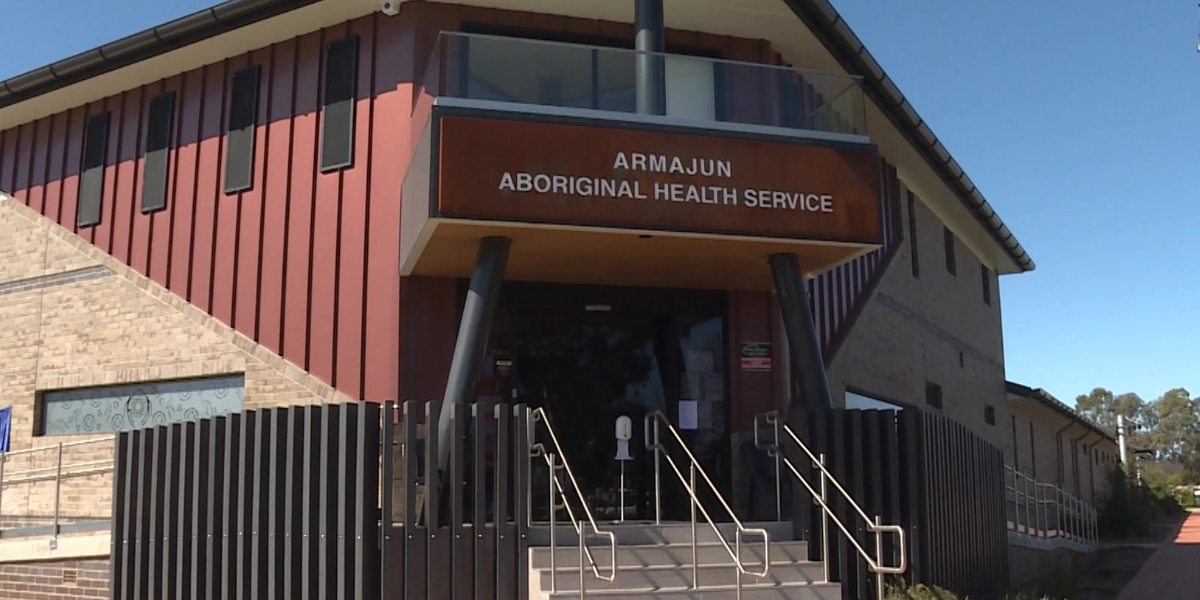
He tried to seek help from the local Aboriginal health clinic but was told the clinic couldn’t prescribe certain pain medication due to clinic policy. His attempts to get an appointment with a local private doctor have been knocked back.
“I can’t get into a doctor, because all the books are full. I’ll have to try Warialda or Glen Innes, but not everyone can afford to take two hours out of their day to go and see a doctor,” he says.
Chronic Pain Australia President Nicolette Ellis says rural and regional Australians have always been negatively impacted by their access to and affordability of health care, but more recently especially those trying to access pain medication.
“Unfortunately, due to the transient nature of regional doctors, many do not feel comfortable continuing to prescribe some high-risk medicines like opioids even if this is assisting with the person’s function and quality of life,”
“We have far too many Australians contacting us on a weekly basis because they can’t find a doctor who will support them and many experience withdrawals and then seek help from emergency departments out of desperation,” she says.
Research shows one in five Australians live with chronic pain. The prevalence of chronic pain is much higher in regional areas.
Ellis believes a blanket response to refuse prescribing opioids or other pain medication is not appropriate.
“Withdrawal from opioids is one of the worst experiences an individual can go through. Most of our members describe this as one of the worst times of their life, they feel helpless and suicidal,” she says.
Beetson has owned property maintenance company for 14 years; while he suffers in pain he’s forced to push through to keep his business operating. But he’s calling more doctors or changes to way some medical clinics operate.
“How many other people are in my situation.”
Armajun Aboriginal Health Service were contacted for comment but did not reply.
Like what you’re reading? Support New England Times by making a small contribution today and help us keep delivering local news paywall-free. Donate now